What is osteoarthritis?
OESTEOARTHRITIS YOU NEED TO KNOW
By, Dr.K.Vijayaraghavan,MD.,FIPM(Germany)
WHAT IS OSTEOARTHRITIS?
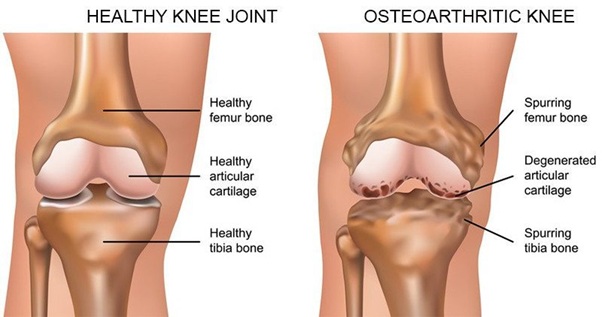
- It is the most common type of arthritis, which can also be known as wear and tear arthritis.
- Important reason is the breakdown or damage to the cartilage between joints.
- The weight bearing joints of the hip, knee and spine are affected in majority of patients.
- Knee pain
- Swelling
- Joint stiffness
- Loss of movement
Causes and Risk Factors
- Age – People above age 45 are at high risk of developing osteoarthritis. However it is mostly found in people over age of 65.
- Gender – It is more common in women above 55 years.
- Obesity – It’s the most common cause of osteoarthritis, as every kilogram puts three extra kilogram of pressure on knees.
- Injury – Joint injury pose an increased risk of developing osteoarthritis.
- Weakness of muscle – Weak thigh muscles lead to osteoarthritis knee joint pain.
Knee Joint Osteoarthritis:
Do’s for Pain Management:
- Use knee cap supports.
- Use hot water fomentation to relieve pain.
- Wear comfortable, fitting shoes to reduce stress on joints.
- Walk regularly to keep yourself active, it helps avoid stiffness.
- Maintain a healthy weight to reduce strain and pain in your knees.
Don’ts for Pain Management:
- Don’t lift heavy weights; it puts stress on the knees.
- Don’t sit cross legged.
- Avoid prolonged activities that put strain on the knee like gardening.
- Avoid jerky movements.
- Don’t smoke. Research shows that smoking leads to joint pain along with other damaging effects.
Healthy eating for osteoarthritis :
- Fuel up on fish
Certain type of fish are packed with inflammation – fighting omega -3 fatty acids, It is recommend to take at least 3 to 4 ounces of fish twice a week. Omega 3- rich fish include salmon,tuna,mackerel and herring is ideal.
- Step up on soy
Not a fan of fish? But still want the inflammation – busting benefits of omega -3 fatty acids? Then try heart-healthy soybeans. Soybeans are also low in fat, high in proteins and fibre and an all-round good-for-you food.
- Don’t Ditch the Dairy
Low-fat dairy products, like milk, yogurt and cheese are packed with calcium and vitamin D, both found to increase bone strength. Vitamin D is essential for calcium absorption, and it has been shown to boost the immune system. If dairy doesn’t agree with you, aim for other calcium and vitamin D rich foods like leafy green vegetables.
- Go Green (Tea)
Green tea is packed with polyphenols, antioxidants believed to reduce inflammation and slows cartilage destruction. Studies also show that another antioxidant in green tea blocks the production of molecules that cause joint damage in people with Rheumatoid Arthritis(RA).
- Grab the Garlic
Studies have shown that people who regularly eat foods from the allium family – such as garlic, onion and leeks – showed fewer sign of early osteoarthritis (OA). Researchers believe that a compound found in garlic may limit cartilage damaging enzymes in human cells.
- Sink Into Some Citrus
Citric fruits – Like oranges, grapefruits and limes – are rich on vitamin C. Research shows that getting the right amount of vitamin aids in preventing inflammatory arthritis and maintaining healthy joints with osteoarthritis(OA).
- Nosh on Nuts
Nuts are rich in proteins, calcium, magnesium, zinc, vitamin E and immune – boosting alpha linolenic acid (ALA), as well as protein and fibre. They are heart-healthy and beneficial for weight loss. Try walnuts, pine nuts, pistachios and almonds.